What is MS?
Multiple sclerosis (MS) is a complex and highly unpredictable disease. In MS, the immune system attacks the central nervous system (CNS) and, over time, wears down the protective cover of the nerves. This permanent damage is called sclerosis. The term multiple sclerosis actually means many scars.
MS fast facts
MS and the body
MS is an autoimmune disease of the CNS, which is made up of the brain and spinal cord, and its course and symptoms vary considerably from person to person.
The immune system normally protects the body against viruses, bacteria and other biological invaders. But in MS, the immune system causes inflammation, or swelling, around blood vessels in the brain and spinal cord and leads to the formation of small, damaged areas called lesions. Although MS can occur at any age, it is commonly diagnosed between the ages of 20 and 49, although onset may be earlier or later.
WHITE BLOOD CELLS
In individuals with MS, white blood cells leave the circulatory system and enter the nervous system, where they are not supposed to be.
DEMYELINATION
When white blood cells encounter nerve cells, they may attack the protective covering of nerve fibres, an area called the myelin sheath.
INFLAMMATION
In MS, both the damage to myelin and nerve fibres and the inflammation weaken the transmission of nerve impulses sent between the brain, the spinal cord, and the rest of the body.
When the brain doesn’t communicate with nerves and muscles the way it is supposed to, the symptoms of MS can occur (like problems with vision, muscle movement, coordination, or balance).
The complex nature of MS
Scientists don’t know the exact cause(s) of MS. However, evidence suggests that lifestyle, environmental, genetic, and biological factors may play a combined role.
The three types of MS and how they may affect the body
In MS, the course of illness and range of symptoms vary from person to person, and there are different types of the disease known as relapsing or progressive types.
With the relapsing types of MS, people experience periods of visible disease activity (relapses) alternating with periods of remission or recovery. Others will experience only a gradual and steady progression of disability, called progressive MS.
There are three types of MS and a condition known as clinically isolated syndrome (CIS).
After a single episode of MS-like symptoms, there may not be enough evidence for a complete diagnosis of MS.
- This is called CIS, and it is typically the first stage of MS.
- Treatment can begin at this stage, before another event occurs.
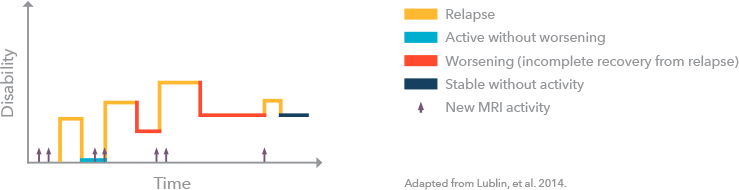
RRMS is the most common type of MS, often seen at first diagnosis.
- RRMS shows clearly defined relapses with some amount of recovery. It affects around 85% to 90% of all people with MS.
- There are periods of relapses or exacerbations (attacks of symptoms) followed by recovery (remission) between relapses. The amount of recovery varies and can be complete or nearly complete.
- Relapses may last as little as 24-48 hours, but the average duration is 8 weeks, but it can be longer or shorter.
- About half of those with RRMS will develop secondary-progressive MS (SPMS) within 10 to 20 years of diagnosis.
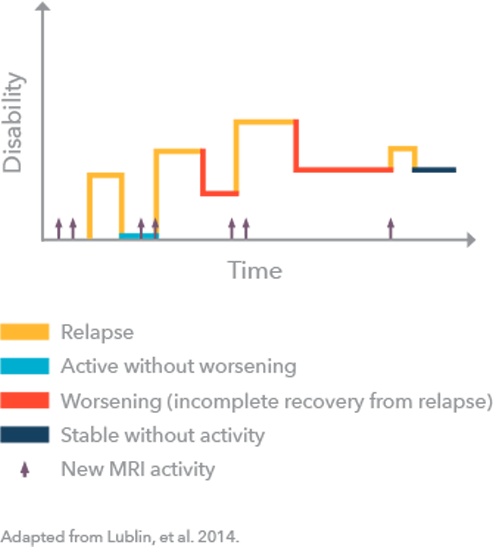
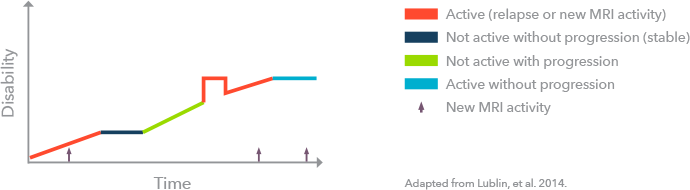
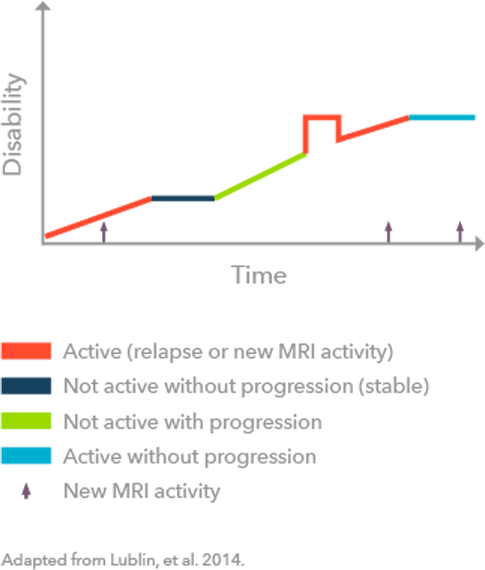
Some people who get diagnosed with RRMS will eventually transition to SPMS, in which there is a progressive worsening of symptoms and disability over time. SPMS is either active (evidence of relapse) or not active, with or without progression (worsening of symptoms).
- While technically a type of progressive MS, SPMS acts more like a relapsing type of MS in its early-to-mid stage, with relapses and remissions being quite common.
- Eventually a more continuous loss of physical and cognitive function starts to take over, and relapses become less common.
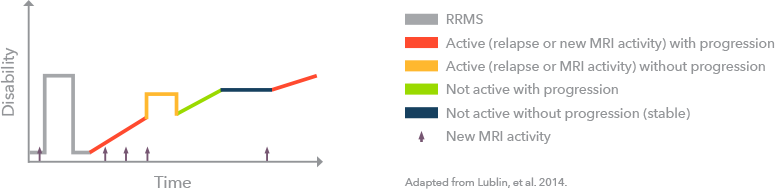
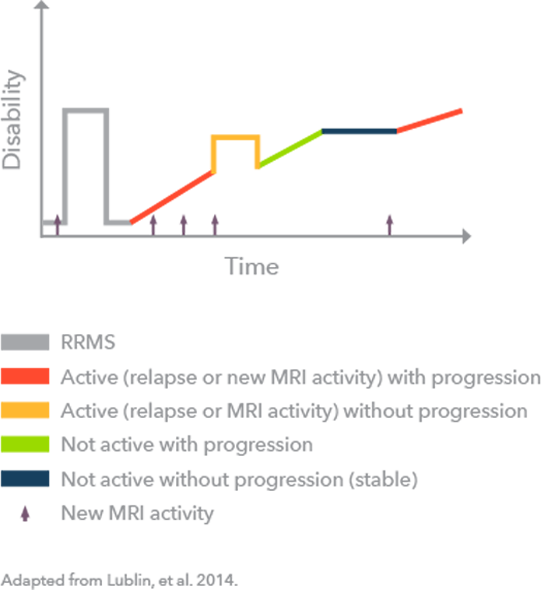
This type of MS affects about 15% of all people with MS and is generally diagnosed after the age of 40.
- This type of MS shows no defined relapses (attacks or flare-ups), but over a period of years, there is a steady, gradual loss of physical and cognitive functions.
- There may be small improvements or plateaus (when the symptoms stay stable), but overall, symptoms tend to get gradually worse.
- People previously diagnosed with a type of MS called progressive-relapsing MS (PRMS) (about 5% of people with MS) are now classified as primary progressive: active (at the time of relapses or new MRI lesions) or not active. The PRMS classification is no longer in use.
Understanding the impact of MS
THE SYMPTOMATIC PROCESS
In early MS, your nervous system usually repairs the myelin damage caused by a relapse (an attack or flare-up).
As MS progresses, your nervous system can repair most of the damage, but not all of it.
Because of this, leftover symptoms accumulate and disability progresses.
RELAPSE FACTS
A relapse means MS is active.
Relapse symptoms are from lesions in the CNS. Relapses are characterized by new symptoms or significant worsening of symptoms. Symptoms depend on the part of the CNS that has been damaged and how badly.
Kim's story
Exploring how MS progresses over time
The symptoms of MS become worse as more nerves become damaged.
The degree of progression varies based on how much nerve damage there is, how quickly it happens, and where it occurs. Research shows that MS continues to progress, even when a person is not having relapses. This happens because MS has two components: the invisible disease and the visible results of it.
The invisible aspect of MS is the ongoing inflammation in the brain and spinal cord. This causes:
SCARRING and LOSS OF NERVE TISSUE
Relapses: Temporary episodes of problems with walking, speech, or vision
Physical disability: Sensory, motor, or other neurological problems that persist or continue to progress
Cognitive dysfunction: Problems with memory and other thinking skills
When MS progresses, disability steadily increases without periods of relapse and remission.
The damage to the nervous system worsens and symptoms become more limiting when MS is untreated.
- MS should be treated as early as possible, even if the disease is in the invisible phase.
- Treating early can help slow the progression of disability and prevent damage from occurring.
- Medicines using interferon have been used to slow the progression of disability in RRMS and SPMS.
If left untreated, RRMS can eventually become SPMS. In SPMS, the level of disability steadily increases without periods of relapse and remission.
Check out the latest articles on current MS topics
Resources
Understanding MS brochure
Stay Informed
Receive email alerts when new articles become available and receive helpful information about MS

